Infertility is the inability to conceive / get pregnant after one year of regular intercourse. One year is the point in time when a medical evaluation is initiated.
However, there are exceptions to this:
1. No periods or irregular periods – immediate workup as woman may not be ovulating.
2. Age over 35 to 40 – 6 months as conception is lower after age 35.
3. Approximately one third of infertility is due to the male, one third due to the female and one third a combination of male and female factors.
Infertility is the inability to conceive / get pregnant after one year of regular intercourse. One year is the point in time when a medical evaluation is initiated.
Infertility is the inability to conceive / get pregnant after one year of regular intercourse. One year is the point in time when a medical evaluation is initiated.
However, there are exceptions to this:
1. No periods or irregular periods – immediate workup as woman may not be ovulating.
2. Age over 35 to 40 – 6 months as conception is lower after age 35.
3. Approximately one third of infertility is due to the male, one third due to the female and one third a combination of male and female factors.
Infertility Evaluation can be completed in one to two months depending on where you are in your menstrual cycle.
1. A test of ovulation – serum progesterone on day 22 of menstrual cycle.
2. Vaginal probe ultrasound to evaluate the uterus and ovaries. The number of small follicle 2-9 mm are counted to estimate ovarian reserve.
3. A test of tubal function:
· HSG – hysterosalpingogram. An x-ray of tubes and uterus to make sure the fallopian tubes are open and the uterus is open. Performed in radiology, after menses and before ovulation.
· Laparpscopy – minor outpatient procedure. The tubes, uterus and ovaries are examined visually, and the tubes are evaluated to make sure they are open. Scar tissue or adhesions and endometriosis can be diagnosed at the time of laparoscopy.
· Femvue – an ultrasound evaluation of tubal patency. Air bubbles are instilled in the uterus and observed to see if they exit the tubes. Performed after menses and before ovulation.
4. Ovarian Reserve – in patients over 35 to 40 years old.
5. Blood tests – Day 3 FSH and estradiol, and AMH on any day of the menstrual cycle.
6. AFC (Antral Follicle Count) – the number of follicles between 2 and 9 mm measured during the vaginal ultrasound exam.
Semen Analysis
Common Causes of Infertility
Common Causes of Infertility
Male
Low sperm counts, low numbers of motile sperm and abnormal sperm can cause infertility.
Sometimes medicine can improve the situation. IUI (intrauterine insemination) and IVF (in vitro fertilization) with ICSI (intracytoplasmic sperm injection or directly injecting the sperm into the egg) can work around the low numbers. With patients with no sperm, sometimes sperm can be retrieved for IVF directly from the testicle. If no method for sperm collection works then donor sperm can be used.
We recommend men with a problem be evaluated by a urologist with special training in infertility.
Female
Can be resolved with oral medicines or injectable hormones.
Tubal Ligation – Tubes can be put back together or IVF.
Blocked Tubes – IVF surgery on blocked tubes not as successful as IVF.
Unexplained Infertility – All tests are normal in both the male and female. Treatment involves either IUI or IVF.
The sperm (semen) specimen is mixed with culture medium and centrifuged to isolate the sperm. The sperm motility is enhanced and then the specimen is placed in the uterus just after ovulation.
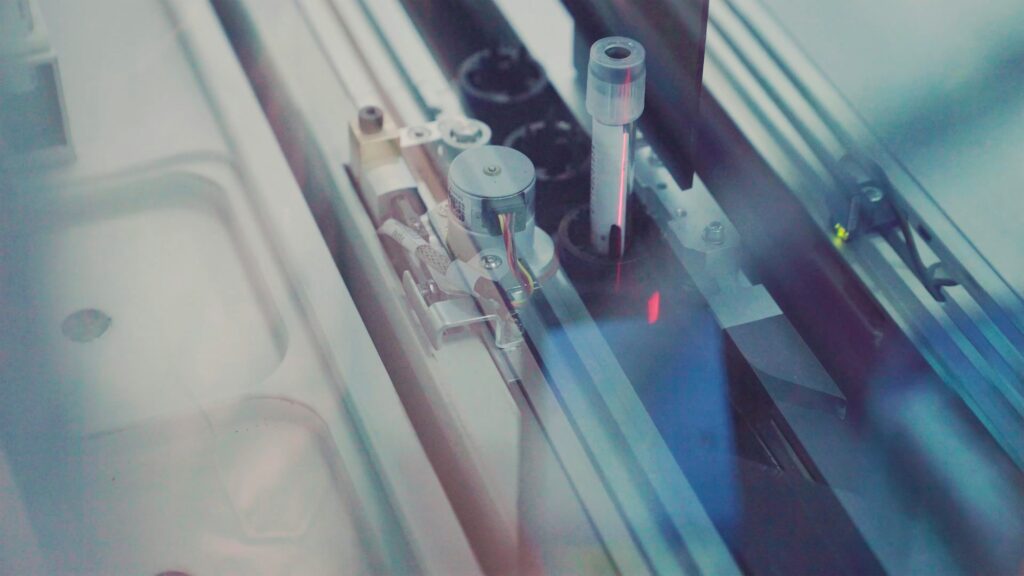
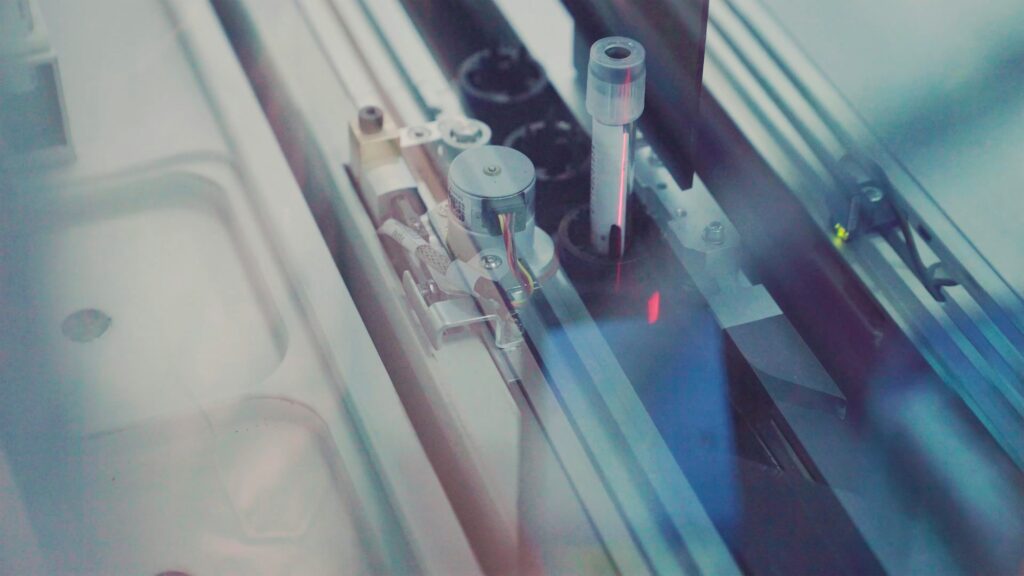
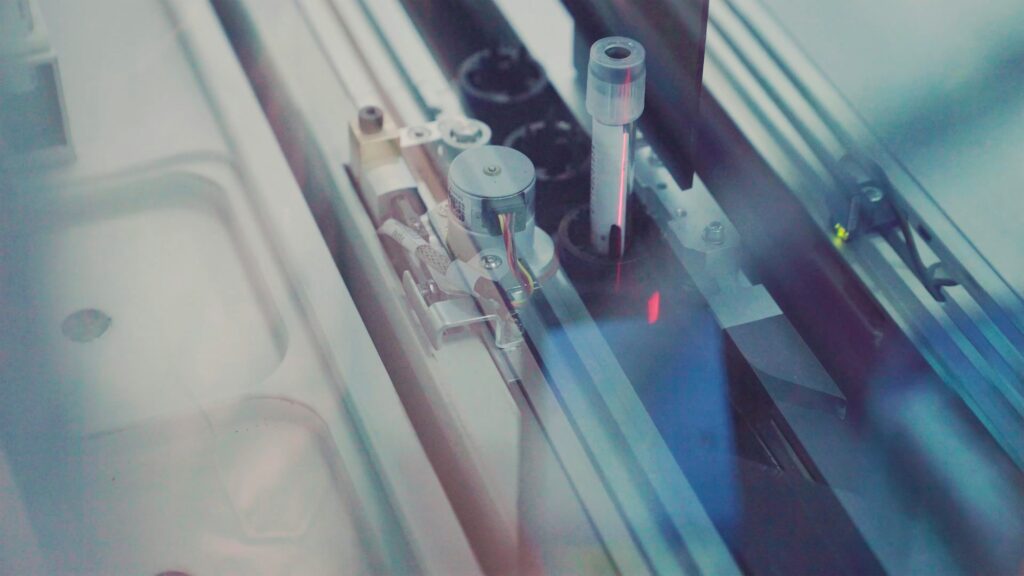
The woman is stimulated (superovulated) with potent hormone injections to obtain as many eggs as possible. The eggs are removed from the ovaries via ultrasound in the clinic under sedation. The eggs are examined and then fertilized with sperm by directly injection the sperm into the eggs (ICSI). The fertilized eggs are then cultured in the laboratory for 4-6 days until they reach the blastocyst stage of development. The area that will develop into the placenta is biopsied and sent to a genetics laboratory for analysis. The blastocyst is then frozen until needed.
Once the genetics are known the most normal embryo is transferred back into the woman. The remaining normal embryos can be transferred during later cycles. Eggs or sperm can be used from anonymous donors and a surrogate can gestate the embryos.
